|
Almost everyone will experience lower back and/or neck pain at some point in their lives, even if just in the form of a slight neck twinge after sleeping in an odd position. Spinal pain of the thoracic region (the upper & middle part of your back) is less common, however you might be surprised to discover how important this part of the body can be when it comes to pain and injury. What is it?
The thoracic region refers to the part of the spine that is surrounded by the rib cage. It consists of 12 vertebrae with discs that sit between each of them. The thoracic spine isn’t an area that you might associate much with movement, however, this area can account for a surprising amount of flexibility, particularly in rotation. With joint attachments both between each side of the 12 vertebrae and a rib on either side, the thoracic spine has almost more individual joints than you can count. If each of these joints is not regularly moved through their full range they can tighten up and lose flexibility. This stiffness can become quite significant over time. Why is it important? Many people may not even notice this lack of movement, primarily because the neck and lower back provide much more range and can usually compensate for any loss of thoracic flexibility to complete everyday tasks. When there is no movement occurring in the thoracic region, this means that the structures of the joints in other regions are pushed closer to their limits of range, particularly during rotation. This results in more compression and stress on these joints and the structures surrounding them, such as nerves, blood vessels and muscles. Thoracic stiffness can be a significant risk factor for neck and lower back pain. This can also reduce the mobility of the chest wall, which can result in less efficient breathing mechanics and, in extreme cases, even reduced exercise tolerance. Thoracic spine movement is aslo important for normal shoulder function, as well as maintaining good posture. How can physiotherapy help? Your physiotherapist is able to assess your thoracic mobility and help you with treatments to improve your range, both with manual therapy and home exercises. They may even help improve your thoracic flexibility as part of a treatment plan for neck and lower back pain.
0 Comments
For most of us, the hours we spend sleeping are simply a time for rest and recovery. However, you might be surprised to learn that your sleeping position can have a significant impact on your body, particularly if you already have an injury. Here are some tips to help to stay pain free overnight. Back pain tips:
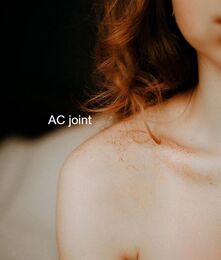
For sufferers of back pain, finding a comfortable position at night can be difficult. The natural curves of the spine need to be maintained and supported throughout the night. Ideally, your body should be held in a position of minimal stress while sleeping. This means that all your joints and muscles are resting in a neutral position A mattress that is too soft might feel comfortable to begin with, but over time will let you sink into it too much, meaning the curve of the lower spine will be lost. Waking up with a stiff or sore back could be a sign that you are using the wrong mattress. A mattress that is too firm can also mean your spine is held in a flattened position, which is both uncomfortable during the night and when you wake up. For many people, sleeping on their side keeps their spine in a more natural alignment than sleeping on their back, especially if they put a pillow between your knees. If you do sleep on your back, placing a pillow under your knees can help to maintain your lumbar spinal curve throughout the night. This can also help to reduce hip and knee pain. Neck pain tips: The neck is often the most vulnerable part of the body if your sleeping setup is not ideal. Side sleepers may let their neck fall excessively to the side with a pillow that is too low or have their neck elevated too much by having their pillows too high. If you find yourself putting your arm under your pillow while you sleep, it is likely that your pillow is too low. Having your shoulder in this position overnight can put unnecessary stress on the structures around the shoulder joint and should be avoided if possible. Stomach sleeping can also put additional pressure on your neck as it is turned to the side for long periods. Hip pain tip: Side sleepers often spend their nights with one leg crossed over their body. This can place extra pressure on the structures on the side of the hip, such as tendons and bursa and can impact the health of these tissues as the compression reduces the blood flow to the area. Placing a pillow under your knee while sleeping on your side in this position can help to maintain a neutral alignment of your hip. Speak to your physiotherapist for more advice on how to improve your sleeping posture and find out if your sleeping setup is right for you. What is it? The AC (acromioclavicular) joint is a thick fibrous joint that connects the top of the shoulder blade to the outer end of the collarbone. The joint is required to be strong and supportive and is the primary way in which weight-bearing forces are transferred from the arm to the rest of the skeleton. The joint is connected by three strong ligaments, the acromioclavicular, corococlavicular and corocoacromial ligaments. How does this injury occur?
The primary mechanism that will cause this joint and its ligaments to be injured is a force that separates the shoulder away from the collarbone, usually in a downwards direction. This can occur from a fall into the ground where the top of the shoulder hits the ground first, a rugby tackle or a fall onto an outstretched hand. As with all injuries, there are many variations in severity and a grading system has been developed to classify AC joint injuries. What are the symptoms? After an AC joint injury, there is usually immediate pain on the top of the shoulder, often with swelling and bruising. There is usually some loss of movement of the shoulder and pain from putting weight through the arm or carrying heavy objects. In severe cases, there is a visible lump on top of the shoulder known as a ‘step deformity’, where an obvious height difference can be seen between the top of the shoulder and the collar bone. There is frequently pain felt when reaching across the body, such as when putting on a seatbelt. To confirm the diagnosis, your physiotherapist can perform some clinical tests and sometimes an X-ray can help to grade the severity of the injury. The classification that would be given to you by your physiotherapist or doctor helps to determine the optimal course of action for each injury. There are different classification systems, some use four grades and the other six. Injuries with a smaller number of ligament fibres being torn are given a lower grade classification, going upwards as further damage is incurred. Injuries classified as higher grades will require surgical repair. How can physiotherapy help? The role of physiotherapy in this case is to ensure the joint is supported and given a chance to heal naturally while maintaining strength and movement of the shoulder girdle. This is done initially by providing support to the joint. You may need to have your arm supported in a sling or brace for some of this time, or your physiotherapist can show you some taping techniques to add support. Most AC joint sprains take around six weeks to fully heal, although some patients report ongoing shoulder problems years later. For this reason, a comprehensive rehabilitation program is very important. More severe sprains or total separations may require surgery to stabilise the joint and treat any associated fractures. Surgical repair will also require a proper rehabilitation program afterwards. The "socket" of the shoulder joint is surrounded by a ring of flexible connective tissue, known as a labrum. This labrum increases the stability of the shoulder while allowing the joint to stay flexible. The long head of the biceps tendon has an attachment directly into the labrum, which is often a point where injuries occur. A tear of the labrum can occur in many locations, however the most common is at the point where the biceps tendon attaches. Usually, this tear follows a typical pattern and is referred to as a superior labrum tear, anterior to posterior (SLAP tear). How do they happen?
SLAP tears can be caused by trauma such as a fall onto an outstretched hand or can develop over time through repeated stress. Repetitive overhead activities such as throwing or painting can also gradually weaken the labrum over time and lead to a tear. What are the symptoms? Often if a SLAP tear develops over time, patients can be unaware they have sustained an injury at all and there is no significant impact on their pain or function. Pre-existing SLAP tears can however place more tension on the long head of the biceps tendon, leading to overuse disorders of that tendon as a secondary complication. When the tear occurs through a sudden action or trauma, symptoms can be more noticeable. Patients often notice pain deep in the shoulder joint with overhead shoulder movements, a feeling of weakness or a loss of power or accuracy with throwing activities. Some people may feel a popping or clicking sensation and occasionally the shoulder feels like it "gives way". In severe tears, the shoulder might feel unstable and be at increased risk of dislocation. How can physiotherapy help? Your physiotherapist can help diagnose a SLAP tear and send you for scans if needed. SLAP tears are graded by severity from 1 to 4 as a way to guide treatment. Physiotherapy is usually recommended as a trial for all tears before considering surgical repair and in many cases can effectively help patients return to their previous activities, symptom free. If physiotherapy is unsuccessful, surgical repair with a full rehabilitation program is then recommended. Surgery will either repair the tear or reattach the biceps tendon to the humerus (tenodesis). Following surgery, a period of rest in a sling is required before rehabilitation can begin. What is it? A broken collarbone, or clavicle, is one of the most commonly broken bones in the body. The clavicle connects the front of the ribcage to the shoulder and is the only bony connection the arm has to the rest of the body. Many muscles attach to the clavicle, including the deltoid and pectoralis Major. How does it happen?
The most common way for this injury to occur is through a fall onto the shoulder. This can happen from a simple fall or sports such as mountain biking or football. It is a common childhood injury but can happen at any age. What are the symptoms? Usually, a broken collarbone will cause moderate to severe pain over the broken area. The patient may have heard or felt a popping or cracking at the time of the injury and there may be an ongoing grinding or creaking with movements of the upper arm. If the skin is not broken there may be bruising and swelling over the painful area. What is the treatment? While very severe cases can be surgically fixed, more often a broken collarbone will be allowed to heal naturally with rest and monitoring. By supporting the arm in a sling and providing pain relief the arm will mend on its own. As with most fractures, there are often other injuries that need to be dealt with at the same time. There are many important structures near the collarbone that can be damaged, including muscles, nerves and blood vessels. In very severe cases, the lung tissue under the collarbone can be damaged causing the lung to collapse. Physiotherapy and recovery: Once a treatment plan has been decided by your medical team, your physiotherapist can help you to return to your pre-injury strength and mobility with a full rehabilitation program. What is the labrum of the shoulder? The shoulder is a remarkably mobile joint, however this flexibility comes with the cost of less stability. The glenohumeral joint, where the upper arm meets with the shoulder blade is a ball and socket type joint. The surface area of the ‘socket’ part of the joint (the glenoid fossa) is much smaller than the ball part of the joint (the head of the humerus). A fibro-cartilaginous ring called a labrum surrounds the edge of the glenoid fossa which acts to increase both the depth and width of the fossa. This labrum provides increased stability and is also the attachment for a part of the biceps muscle via a long tendon. The labrum can provide flexibility and stability that a larger glenoid fossa might not be able to, however being a soft structure it is prone to tearing which can be problematic. What causes the labrum to tear?
The most common way the labrum is torn is through a fall onto an outstretched arm or through repetitive overhead activities such as throwing or painting, as the repeated stress on the labrum can cause it to weaken and tear. Suspected labral tears can be diagnosed in a clinic by your physiotherapist through a series of tests, however, an MRI is usually required to fully confirm the presence of a labral tear. Labral tears are classified into different grades, which are determined by their location and severity. This grading is used as a guide to help determine the correct treatment. What are the symptoms of a labral tear? A labral tear is often associated with other injuries, such as a rotator cuff tear, which can make the clinical picture a little confusing. Commonly there will be pain in the shoulder that is difficult to pinpoint and the pain will be aggravated by overhead and behind the back activities. Severe labral tears can lead to instability and can also be related to dislocations of the shoulder. How Can Physiotherapy Help? The severity and grade of the labral tear will guide treatment. Smaller tears can be treated with physiotherapy that is aimed at increasing strength and control of the shoulder. Other tears may require surgical repair after which physiotherapy is an important part of treatment to rehabilitate the shoulder. Tendons, the connective tissues that join muscles to bone are known for being notoriously difficult to treat once injured. The reason for this is that often they are injured through stress or overuse, and compared to muscles they can have relatively poor blood flow, which is essential for healing. Tendons and muscles work together to move your joints and together are called a contractile unit. As muscles are exercised and gain strength, the attaching tendons are also placed under tension and adapt to this to become stronger. If the load placed on the tissues exceeds their capacity, the tendon fibres can begin to break down and become stiff and painful. Is my pain related to a tendon injury?
For an accurate diagnosis, you will need to be assessed by a physiotherapist. However, some signs that your pain might be coming from an in issue with a tendon are; · The pain is quite specific and can be felt over the tendon itself; · The pain is worse when under stress and improves when rested; · The pain improves after exercise has started, but it might be worse once you cool down; · The area around the tendon may feel stiff after periods of rest, particularly in the morning. How are tendon injuries treated? When it comes to recovery, tendons are often treated differently to other injuries. While each tendon injury is unique and will require assessment and intervention by a physiotherapist, there are a few general approaches that usually help with all tendon injuries. Reducing your activity to a comfortable level is the first step to recovery. Complete rest can actually delay healing as the tendon simply becomes weaker and less able to cope with subsequent loads. Your physiotherapist can provide you with a targeted exercise program to aid your recovery. Eccentric exercises, which are exercises that work alongside gravity, have been shown to stimulate tendon healing and strength. Stretching may aggravate your injury and should be used with caution. Assessment of any biomechanical faults or stresses that are placing undue load on the tendon is also a central component of treatment. Your physiotherapist is able to guide you with your recovery and return to sport to avoid aggravating any injury. The shoulder is a fascinating joint with incredible flexibility. It is connected to the body via a complex system of muscles and ligaments. Most of the other joints in the body are very stable, thanks to the structure of the bones and ligaments surrounding them. However, the shoulder has so much movement and flexibility that stability is reduced to allow for this. Unfortunately, this increased flexibility means that the shoulder is more vulnerable to joint dislocations. What is a dislocation and how does it happen?
As the name suggests, a dislocated shoulder is where the head of the upper arm moves out of its normal anatomical position to sit outside of the shoulder socket (the glenoid). Some people have more flexible Joints than others and will, unfortunately, have joints that move out of position without much force. Other people might never dislocate their shoulders unless they experience a traumatic injury that forces it out of place. The shoulder can dislocate in many different directions, the most common being anterior or forwards. This usually occurs when the arm is raised and forced backward in a ‘stop sign’ position. What to do if this happens The first time a shoulder dislocates is usually the most serious. If the shoulder doesn’t just go back in by itself (spontaneous relocation), then someone will need to help to put it back in. This needs to be done by a professional as they must be able to assess what type of dislocation has occurred, and an X-ray may need to be taken before the relocation happens. A small fracture can also occur as the shoulder is being put into place, which is why it is so important to have a professional perform the procedure with X-Ray guidance if necessary. How can physiotherapy help? Following a dislocation, your physiotherapist can advise on how to allow the best healing for the shoulder. It is essential to keep the shoulder protected for a period to allow any damaged structures to heal as well as they can. After this, a muscle strengthening and stabilization program can begin. This is aimed at helping the muscles around the shoulder to provide optimum stability and prevent future dislocations. The information in this article is not a replacement for proper medical advice. Always see a medical professional for an assessment of your condition. What is it? Shoulder instability is a term used to describe a weakness in the structures of the shoulder that keep the joint stable, which can lead to dislocation. As one of the most mobile joints in the body, the shoulder maintains stability through a balance of support between the dynamic structures (muscles and tendons) and static structures (ligaments and joint shape). Shoulder instability most often occurs in one of two directions, anterior (forward) or posterior (backwards). Anterior instability or dislocations are more common than posterior. What are the symptoms?
The most noticeable symptom of shoulder instability is dislocation or subluxation of the joint. This is often accompanied by pain, clicking sensations, a feeling of instability and in some cases weakness, and pins and needles in the arm. Many patients report a feeling of apprehension or instability, as if ‘something is not quite right’. Posterior instability can also cause reduced range of movement and might mimic other common shoulder conditions, which need to be ruled out first. How does it happen? Shoulder instability can be classified as traumatic, occurring after an injury or atraumatic, where the shoulder is exceptionally flexible and prone to dislocations from everyday forces. Instability can also occur from chronic overuse where the shoulder joint is damaged slowly over time. Traumatic shoulder instability is the most common form. Often the joint is dislocated by a strong force and damaged, leaving it more unstable and vulnerable to future dislocations. Rugby and football players are commonly affected. However, dislocations can occur in the general public from something as simple as falling onto an outstretched hand. How can physiotherapy help? Shoulder instability is a complex condition and each person will have a different combination of causes and structural deficiencies. Physiotherapists are trained to identify issues of coordination, control and strength that may be contributing to instability and provide an extensive rehabilitation program. For some patients, surgery is recommended to help restore some static stability to the joint. However, this is not the best pathway for everyone. If surgery is indicated, a full rehabilitation program is recommended post-operatively for the best possible outcome. Helping patients to understand and manage their condition is an essential part of recovery. Physiotherapy is usually recommended as the first line of treatment before surgery and can have excellent outcomes, with or without going under the knife. |
Categories
All
|